Overview
All victims of sexual assault should be able to access clinical care focused on their medical wellbeing. This includes timely and responsive forensic medical examinations to support investigations and potential prosecution, where there is consent.
In our previous audit, Delivering forensic services (Report 21: 2018–19), we found opportunities for Queensland Health to improve its statewide all-hours clinical and forensic care services. We did not follow up all recommendations from our 2018–19 report, including those related to deoxyribonucleic acid (DNA), as the government announced changes as a result of the inquiry into forensic DNA testing in Queensland.
In addition to our report, there have been several other reviews and inquiries into Queensland Health’s delivery of forensic medical services to victims.
Tabled 27 September 2024.

Report on a page
All victims of sexual assault should be able to access clinical care (which is focused on their medical wellbeing and health) and forensic medical examinations (which gathers forensic medical evidence to support an investigation and potential prosecution) that are timely and responsive to their needs.
Queensland Health has a statewide all-hours service to provide sexual assault victims with clinical and forensic care and support. In June 2019, in our audit Delivering forensic services, we found opportunities to improve these services. This audit examines whether Queensland Health has effectively planned and progressed implementing recommendations and directions to improve the delivery of forensic medical examinations. These include:
- recommendation 4 from our report Delivering forensic services (Report 21: 2018–19)
- recommendations 32 to 37 from the Women’s Safety and Justice Taskforce (the Taskforce) Hear her voice – Report two
- the Ministerial Direction – Crisis Care Process issued by the Minister for Health, Mental Health and Ambulance Services and Minister for Women on 17 November 2023.
We did not follow up the other recommendations from our 2018–19 report, including those related to deoxyribonucleic acid (DNA) testing. The government announced changes resulting from the 2022 Commission of Inquiry into Forensic DNA Testing in Queensland, which meant it was not an appropriate time for us to follow up on related recommendations.
Queensland Health continues to improve its services
Queensland Health has continued to improve the services that it delivers to victims of sexual assault since our 2018–19 report. It now has service delivery agreements with each hospital and health service (HHS), new forensic medical examination kits, and new reporting pathways for victims. It has fully implemented 4 of the 6 recommendations made by the Taskforce and is continuing to implement the remaining 2 recommendations. It still needs to implement an overall strategy to ensure there are enough forensic medical examiners across the state, enhance its monitoring and reporting, and increase the availability of paediatric services for child victims.
There is a greater focus on providing early clinical care to victims
The Crisis Care Process ministerial direction issued in November 2023 requires 13 of the 16 HHSs (those with the most emergency department presentations) to ensure victims of sexual assault start receiving clinical care within 10 minutes of presenting to hospital. The direction appears to have prompted HHSs to prioritise more timely care to victims. HHSs have adopted differing practices in the clinical care they provide to victims across the state. This is reasonable, as practices need to differ based on the specific medical needs of the victim and the clinical judgement of those providing care. Queensland Health is implementing a new reporting framework to improve consistency in the information HHSs capture and monitor whether they are complying with the direction.
Queensland Health does not know how many victims experience delays obtaining forensic medical examinations
We found instances where some victims could not obtain a timely forensic medical examination. However, an absence of data meant we could not determine how isolated these instances are. Queensland Health acknowledges that gaps still exist in its service for some victims. It plans to implement new frameworks and use the $56 million announced in the 2024–25 state budget to recruit more dedicated forensic medical examiners. In this report, we make 3 further recommendations to improve the clinical care and forensic medical examinations that Queensland Health provides to victims of sexual assault.

Audit conclusions
Queensland Health has improved the services it delivers to victims of sexual assault since our 2018–19 report. It has implemented most of the recommendations we and the Women’s Safety and Justice Taskforce made, and the Crisis Care Process ministerial direction. It introduced service delivery agreements with each hospital and health service (HHS), new forensic medical examination kits, and new reporting pathways for victims. It has also trained more than 400 doctors and nurses in how to perform forensic medical examinations since July 2023. It has undertaken these reforms while responding to, and recovering from, a global pandemic.
The Crisis Care Process ministerial direction was issued in November 2023. At the time of undertaking this audit, the Minister for Health, Mental Health and Ambulance Services and Minister for Women had only recently issued the direction. While still early in its implementation, indications from hospital staff suggest it has prompted HHSs to prioritise more timely care to victims of sexual assault. Queensland Health relies on HHSs to self-report if they fail to comply with the direction. It has recently developed a reporting framework, and is currently enhancing its systems to better track whether HHSs are complying with the direction.
There is more Queensland Health can do to further improve its services. While it has addressed most elements of recommendation 4 from our 2018–19 report, it still needs to expand the availability of paediatric services for child victims. (That recommendation focused on developing and delivering reforms to improve services to victims – see Appendix C.). In June 2024, it committed $12 million to enhancing paediatric services for child victims.
It has fully implemented 4 of the 6 recommendations made by the Women’s Safety and Justice Taskforce (the Taskforce – an independent group set up by the Queensland Government). It has partially implemented the remaining 2 recommendations. In July 2022, the Taskforce recommended a new statewide forensic examination service be established with dedicated forensic medical examiners. Queensland Health’s existing service relies on a mix of dedicated forensic medical examiners and trained doctors and nurses (including emergency department doctors and nurses), supported by a statewide phone service. Given the existing pressure on emergency departments, HHSs must balance these competing medical priorities. Queensland Health could better understand the overall demand for forensic medical examinations across HHSs to aid it in developing effective strategies to address any service gaps. This is particularly important in rural and remote areas.
Queensland Health can provide greater oversight of the delivery of forensic medical examinations, to ensure they are both timely and responsive to a victim’s needs. It has not developed reporting tools to capture when a victim commences an examination, the reasons for any delays, and the quality of forensic samples taken. Doing so would enhance the accuracy and completeness of its data, which it could then use to benchmark performance, help improve care, and drive efficiencies.
Queensland Health acknowledges there are still gaps in how it provides clinical care and forensic medical examinations to victims of sexual assault. To address these gaps, it plans to implement new frameworks for sexual assault care and performance reporting. It also plans to recruit more dedicated forensic medical examiners across the state using the funding announced in the state budget.

Recommendations
| Improving early clinical care for victims (Ministerial Direction – Crisis Care Process) |
We recommend Queensland Health: 1. implements its performance reporting framework to ensure victims of sexual assault are provided with timely and professional clinical care (Chapter 2) in accordance with the Ministerial Direction – Crisis Care Process. This should include:
|
| Building capability to deliver statewide forensic medical examination services |
We recommend Queensland Health: 2. ensures suitably trained forensic medical examiners are available across the state to provide timely forensic medical examinations to victims of sexual assault (Chapter 3). This should include:
|
| Monitoring and reporting the delivery of forensic medical examinations |
We recommend Queensland Health: 3. improves its monitoring and reporting of the performance of HHSs in delivering forensic medical examinations to victims of sexual assault (Chapter 3). This should include:
|
Reference to comments
In accordance with s. 64 of the Auditor-General Act 2009, we provided a copy of this report to relevant entities. In reaching our conclusions, we considered their views and represented them to the extent we deemed relevant and warranted. Any formal responses from the entities are at Appendix A.

1. Context: forensic medical examinations for sexual assaults
Sexual assault in Queensland
As of September 2024, the number of reported sexual offences in Queensland has increased by 57 per cent in the last 6 years, rising from 6,745 cases in 2017 to 10,557 cases in 2023.
Sexual assault is a particularly degrading crime. The impact to victims can be physical, emotional, psychological, and long lasting.
Forensic medical examinations
All victims of sexual assault should be treated with respect and compassion. They should be able to access clinical care (which is focused on their medical wellbeing and health) and forensic medical examinations (focused on gathering forensic medical evidence to support an investigation and potential prosecution) that are timely and responsive to their needs. The victim’s health and wellbeing take priority over the need for gathering forensic medical evidence.
A victim who reports a sexual offence to police or attends a hospital may be asked to undergo a forensic medical examination. They have a choice, and must give their consent for the examination to occur.
The primary purpose of a forensic medical examination is to document injuries and collect forensic samples (such as swabs) for potential use as evidence in a criminal investigation and prosecution.
It is an intrusive process that can be confronting and distressing for victims. Many are in a very fragile and distraught state, often still wearing the clothing they were assaulted in. The examinations need to be performed professionally to reduce the likelihood of exacerbating the victim’s trauma, and to allow other specialist services, such as counsellors, to begin supporting the victim. The examinations must also be timely, to preserve forensic evidence that can deteriorate over time.
A doctor or sexual assault nurse examiner (collectively referred to as a forensic medical examiner) uses a forensic medical examination kit to collect DNA evidence. The examination typically takes between one to 3 hours. The evidence collected is sent to a Queensland Health laboratory, where a forensic scientist analyses it to identify any DNA. The evidence may be presented in court.
Reforms relating to forensic medical examinations
Reviews, audits, and inquiries
Over the past 6 years there have been several reviews and inquiries into Queensland Health’s delivery of forensic medical examinations for victims of sexual assault. They include our previous audit, Delivering forensic services (Report 21: 2018–19). They have found a range of shortcomings in the care provided to victims of sexual assault and in the timeliness and appropriateness of forensic medical examinations. Appendix C provides more detailed information about our 2018–19 report and the Women’s Safety and Justice Taskforce Hear her voice – Report two and their recommendations.
Figure 1A shows a timeline of key reviews and events related to the delivery of forensic medical examinations from 2019 to 2024.

Queensland Audit Office using information provided by Queensland Health.
Statewide reforms
In January 2019, Queensland Health began reforms to forensic medical examinations. This included:
- drafting a health service directive requiring hospital and health services to deliver forensic medical examinations
- delivering forensic medical examination training to doctors and nurses statewide.
Who is responsible for forensic medical examinations?
The Department of Health (the department) is responsible for the policy, framework, strategy, and training for forensic medical examinations. The 16 hospital and health services (HHSs) are responsible for carrying out the examinations for victims. In this report, we refer to the department and the 16 HHSs collectively as Queensland Health.
Entities such as the Queensland Police Service and the Department of Justice and Attorney-General (DJAG) also play an important role. The Queensland Police Service is responsible for investigating instances of sexual assault and helping to transport forensic evidence. DJAG is responsible for the administration of the Queensland courts.
In July 2024, Forensic Science Queensland (previously called Forensic and Scientific Services), which is responsible for the analysis of forensic evidence, was transferred from Queensland Health to DJAG.
Several non-government organisations provide support to victims of sexual assault.
What did we audit?
This follow-on audit examines whether Queensland Health has effectively acted on recommendations and directions designed to improve the delivery of forensic medical examinations for victims. This includes:
- recommendation 4 from Delivering forensic services (Report 21: 2018–19) directed to the Department of Health
- recommendations 32 to 37 from the Women’s Safety and Justice Taskforce’s Hear her voice – Report two directed to Queensland Health.
Recommendation 38 from the Taskforce recommended that the Queensland Audit Office consider undertaking a follow-up audit of our 2018–19 audit and review the implementation of the recommendations made by the Taskforce – those relevant to forensic medical examinations.
We also examined Queensland Health’s progress in implementing the Ministerial Direction – Crisis Care Process issued by the Minister for Health, Mental Health and Ambulance Services and Minister for Women on 17 November 2023.
We included the Department of Health and 4 HHSs (Gold Coast, Metro North, Children’s Health Queensland, and North West) in the scope of this audit. We also consulted with other HHSs as part of this audit to seek their views on the delivery of forensic medical examinations.
We did not follow up the other recommendations from our 2018–19 audit. This is because the government has announced changes to forensic DNA testing in Queensland resulting from the 2022 Commission of Inquiry. It was therefore not an appropriate time for us to follow up on related recommendations. We may assess progress on them in future.

2. Providing timely and professional clinical care
On 17 November 2023, the Minister for Health, Mental Health and Ambulance Services and Minister for Women (the minister) issued a direction to relevant hospital and health services (HHSs) to ensure victims of sexual assault ‘commenced a clinical care pathway’ within 10 minutes of presenting to a hospital.
In this chapter, we cover whether Queensland Health has effectively acted on the minister’s direction.
Are victims receiving clinical care within 10 minutes?
The 17 November 2023 Ministerial Direction – Crisis Care Process (the direction) requires HHSs to:
'… accept care and commence an approved Clinical Care Pathway for any person who attends at an Emergency Department and discloses having experienced sexual assault, or is presented by an officer of the Queensland Police Service as a victim of a sexual assault, within 10 minutes of the disclosure or presentation.'
(See Appendix D for the full direction.)
The direction applies to 13 of the 16 HHSs. The department advised that the 13 HHSs included are those with the top 26 reporting public hospitals in Queensland (those that have the most emergency department presentations). It excludes South West, Central West, and Torres and Cape HHSs. While these HHSs have fewer emergency department presentations, it may result in a potential gap in clinical care for victims in these areas. Queensland Health could provide greater guidance as to what it considers would be a reasonable time frame that victims in these areas can expect clinical care to commence within.
The 4 HHSs that we audited reported implementing the direction. We did not audit the other 9 HHSs.
The minister issued the direction after being informed that several HHSs were unable to provide a woman with timely care following an alleged sexual assault. Case study 1 provides more detail on this.
| Several hospital and health services were unable to provide a victim of sexual assault with timely care |
|---|
On the afternoon of 13 November 2023, a woman attended a police station alleging that she had been sexually assaulted. That evening, police contacted the local hospital to arrange a forensic medical examination, but were advised that there was no examiner on shift until the following morning. The police subsequently contacted 3 other hospitals in South East Queensland but were informed the hospitals had no capacity to perform the forensic medical examination until the next day. Late that evening, the police contacted Forensic Medicine Queensland’s 24/7 phone service but were unable to get through, as the staff member was on another call. The victim was subsequently sent home for the night. The next morning, she presented at the local hospital and a doctor began the forensic medical examination. Delays like these can have a significant impact on victims. Not only can they re-traumatise the victim, but they can lead to forensic evidence being lost or degraded. |
Queensland Audit Office using information provided by Queensland Health.
Further guidance for hospital and health services would be helpful
The minister’s direction requires HHSs to commence an approved clinical care pathway, but does not define what that means. Therefore, each HHS must document and approve what it means.
As a result, HHSs across the state have adopted differing practices. Some deem that a victim has commenced clinical care if a social worker has seen them. Others require a nurse or doctor to start basic wellbeing checks, such as taking their blood pressure.
HHS practices differ based on their staffing levels, models of care, and availability of support services. Furthermore, clinical care will differ based on the specific medical needs of the victim and the clinical judgement of those providing care. Nevertheless, there is an opportunity for Queensland Health to provide greater guidance for HHSs to assess and benchmark their compliance and performance against the direction.
The ministerial direction has put greater focus on the importance of early care for victims
The doctors and nurses we spoke to reported that the direction appears to have improved the initial care that victims of sexual assault receive. They reported that it has reinforced to hospital boards the importance and priority of providing timely care to victims.
We were unable to verify whether the direction has improved the initial clinical care provided to victims due to an absence of data.
Queensland Health has limited information on whether the direction is being met
Queensland Health relies on HHSs self-reporting if they fail to comply with the direction. As of 16 August 2024, HHSs reported that there were 49 instances where they failed to ensure victims commenced a clinical care pathway within 10 minutes of presenting to a hospital. Given HHSs are required to self-report this data, we do not know if more HHSs have failed to comply with the direction, and not reported it.
Queensland Health has developed a performance reporting framework and reporting tools to help monitor HHS compliance with the direction. It plans to implement these by December 2025. This is important and will give it greater oversight.
Recommendation 1 We recommend Queensland Health implements its performance reporting framework to ensure victims of sexual assault are provided with timely and professional clinical care in accordance with the Ministerial Direction – Crisis Care Process. This should include:
|

3. Performing forensic medical examinations
In June 2019, in our audit Delivering forensic services (Report 21: 2018–19), we found some victims of sexual assault were refused a forensic medical examination, or experienced lengthy delays. We recommended that the Department of Health (the department) continue to develop and deliver the reforms (that it commenced in January 2019) to forensic medical examinations to improve services for victims.
This included:
- implementing service agreements with hospital and health services (HHSs) to deliver forensic medical examinations
- developing strategies to recruit and retain appropriately trained physicians and nurses
- implementing a range of reporting pathways and supporting processes for all victims
- improving clinicians’ awareness of reporting options for victims of sexual assault
- improving the availability of, and access to, paediatric services for child victims
- establishing interagency services to better integrate doctors and nurses, police, and non-government organisations.
In July 2022, the Women’s Safety and Justice Taskforce (the Taskforce) published similar findings about forensic medical examinations for sexual assault victims. It made 6 recommendations to Queensland Health about establishing and funding a statewide 24/7 forensic medical examination service, and implementing ongoing competency-based training for doctors and nurses. It recommended that the Queensland Government fund this.
In this chapter, we examine whether Queensland Health (which includes the Department of Health and the 16 hospital and health services) has effectively acted on recommendations.
Appendix C contains a full list of the recommendations we have followed up. It also shows our assessment of Queensland Health’s progress against each recommendation.
Can victims of sexual assault access timely and high‑quality forensic medical examinations?
All victims, regardless of where they live, should be able to access timely and high-quality forensic medical examinations. The lack of sufficiently trained and capable forensic medical examiners across the state has been a key focus of various recommendations over the past 5 years.
Queensland Health continues to improve the services it delivers to victims
While Queensland Health has made progress improving its services statewide, more work is needed to ensure all victims can access a timely forensic medical examination, regardless of where and when they require it.
Gap and needs analysis
In response to the Taskforce’s recommendations, Queensland Health commissioned a gap and needs analysis to inform the design of forensic medical examination services across the state. In September 2023, it found that more than half of the 16 HHSs across the state had no dedicated forensic medical examiners.
It also found the health system:
- provides no statewide model of care for victims requiring a forensic medical examination
- lacks a statewide governance structure to oversee service delivery
- does not offer comprehensive or consistent training
- has no formal paediatric statewide support. As a result, some child victims of sexual assault cannot access specialised services tailored to their needs.
The department accepted in principle the 7 recommendations resulting from the gap and needs analysis.
Limitations with the existing staffing approach
HHSs across the state have adopted different staffing models for forensic medical examinations. Some employ doctors and trained nurses specifically for this purpose. Others rely solely on their emergency department doctors and trained nurses to perform these examinations in addition to their existing responsibilities. Some use a mix of both.
Any doctor can perform a forensic medical examination regardless of whether they have been trained. However, all nurses must be trained prior to performing an examination. The department provides support, through a 24/7 phone service, to support emergency department doctors and trained nurses when they are performing forensic medical examinations.
Some HHSs report their emergency department doctors are reluctant to perform forensic medical examinations due to the amount of time it takes, including the time to prepare for and present in court. They said the additional workload can be challenging for staff, and can result in fatigue. Also, they potentially may be required to testify in court, which can be daunting.
The benefits of having dedicated forensic medical examiners
Several HHSs that have employed dedicated forensic medical examiners told us their staffing model has a range of benefits, including:
- better workforce planning
- more timely access to forensic medical examinations for victims
- less pressure on their emergency departments.
This staffing model can come with funding costs for HHSs. Australian research published in the Journal of Forensic and Legal Medicine in May 2013 found the conviction rate was 25 per cent higher for forensic medical examinations performed by qualified forensic medical examiners than it was for those performed by an emergency department or general practitioner doctor.
The research also found that victims felt more confident going to a qualified expert as opposed to their general practitioner or an emergency department.
Lack of paediatric services for child victims of sexual assault
In Delivering forensic services (Report 21: 2018–19), we found there was a lack of paediatric services for child victims of sexual assault. A trained paediatrician has the specialised skills required to examine a child who has been sexually assaulted.
At the time, we found 4 instances where children had issues in obtaining timely and appropriate forensic medical examinations. We recommended the department improve the availability of, and access to, paediatric services for child victims.
The department has taken limited action to improve paediatric services for child victims. In June 2024, it committed $12 million (of the $56 million announced in the 2024–25 state budget) to enhance paediatric services for child victims. In addition, Children’s Health Queensland HHS has delivered some training to doctors that will likely deliver paediatric services to child victims.
Queensland Health needs better visibility of the number of active and dedicated forensic medical examiners across the state
While all doctors in Queensland can perform forensic medical examinations, Queensland Health does not know how many active and dedicated examiners there are. This is the number of trained doctors and nurses that are currently performing examinations. It does not have the systems to record or track the number of active examiners at each HHS. This limits its ability to plan its workforce and ensure there is adequate coverage, particularly during times where emergency departments are experiencing significant pressure. The HHSs we spoke with reported a shortage across the state, particularly in regional and remote areas. This was consistent with the findings from Queensland Health’s gap and needs analysis.
Also, while it has acted to increase the number of qualified forensic medical examiners by delivering more training, it has no strategies in place to retain those already qualified. Neither the department nor HHSs offer any incentives to doctors and nurses to carry out this role.
What is Queensland Health doing to address the gaps?
Queensland Health acknowledges it has gaps in its services statewide and that it sometimes struggles to provide victims with trauma-informed care.
Trauma-informed care recognises and responds to the signs, symptoms, and risks of trauma to a victim. It provides care tailored to the victim’s needs and avoids services that may inadvertently re-traumatise the victim.
To address these gaps, it is developing:
- a statewide framework for sexual assault care
- a performance reporting framework
- an implementation plan.
It plans to implement the new frameworks by December 2025.
In the 2024–25 state budget, the Queensland Government committed $56 million over 4 years to ensure victims of sexual assault have access to timely and high-quality forensic examination services.
Queensland Health does not know how many victims experience delays obtaining forensic medical examinations
Queensland Health does not monitor whether hospitals are delivering timely forensic medical examinations to victims of sexual assault. As such, it does not know how the hospitals carry out the examinations or whether victims continue to experience lengthy delays in waiting for them.
Only one of the 4 HHSs we audited has recorded the time it took to begin a forensic medical examination. Between January and March 2024, it took an average of 3 hours to do this after a victim presented. In one case, a patient had to wait 9 hours at a hospital before a doctor started the forensic medical examination. This was due to staffing shortages.
Due to limitations with the HHS data, we could not determine if this was an isolated case.
Queensland Health needs to work with HHSs to ensure they capture the time at which they start clinical care and the time they begin the forensic medical examination. As well as allowing Queensland Health to understand the timeliness of hospitals in providing care to sexual assault victims, it could also help identify bottlenecks, improve care, and drive efficiencies.
Do doctors and nurses receive adequate training and support to deliver forensic medical examinations?
In Delivering forensic services (Report 21: 2018–19), we found one of the main reasons hospital staff refused to conduct examinations was the absence of trained doctors and nurses. We recommended the department develop strategies to recruit and retain appropriately trained doctors and nurses for forensic medical examinations across the state.
The Taskforce also found only a limited number of doctors and nurses in emergency departments had been trained to perform forensic medical examinations, including in rural, regional, and remote locations. It recommended that Queensland Health develop and implement ongoing competency-based training and professional development for doctors and nurses who may be required to prepare reports and give evidence in court. This included educating doctors about the importance of their role.
In response to these recommendations, Queensland Health has delivered workshops and online training to better educate forensic medical examiners about their responsibilities and the importance of the part they play.
Queensland Health has improved the training it provides to examiners
Between July 2023 and August 2024, Queensland Health has delivered forensic medical examination education and training to 440 doctors and nurses.
Prior to July 2023, it delivered training to examiners but did not record details about the training, including how many doctors and nurses attended.
The education and training involves a 32-hour online course and an 8-hour face-to-face workshop. It covers:
- the responsibilities of a forensic medical examiner and the importance of the role
- how to obtain consent and perform a forensic medical examination
- reporting options for victims of sexual assault
- how to assist with the ongoing management of a sexual assault
- how to prepare a court report.
Forensic medical examiners need more support in preparing for court
Some forensic medical examiners have never been to court before, and may not be aware of the specific legal procedures they need to follow. Some examiners told us that they need more opportunity to present evidence in a simulated courtroom. Queensland Health is working to address this gap. In June 2024, Queensland Health, in collaboration with the Office of the Director of Public Prosecutions, delivered training to 29 doctors and nurses on appearing as an expert witness in a criminal trial and ran mock court trials for forensic medical examiners. Queensland Health intends to deliver this training in South East Queensland biannually. At this stage, there is no intention to run this training in other areas across the state.
Queensland Health needs to provide more training in regional and remote areas
Since July 2023, Queensland Health has run 28 forensic medical examination education and training workshops across the state.
Figure 3A highlights the number of participants who attended the training from each HHS between July 2023 and August 2024.
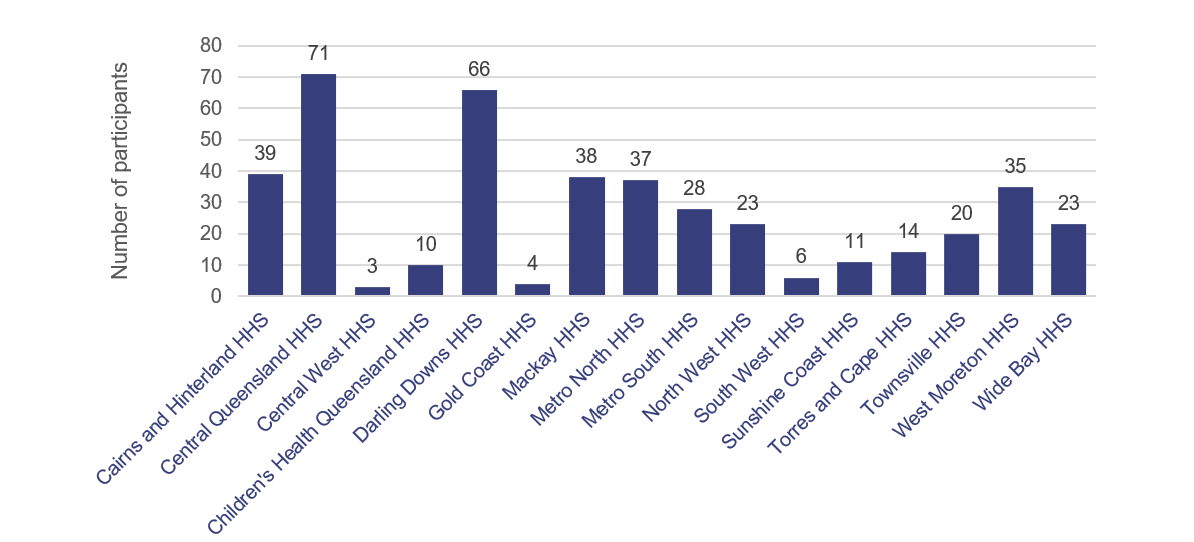
Notes: HHS – hospital and health service. Figure 3B shows the 428 participants that have been trained across HHSs since July 2023. An additional 12 staff have been trained in the Department of Health.
Queensland Audit Office using information provided by Queensland Health.
A total of 440 participants have attended the training. No workshops were held in the Torres and Cape or Central West areas. HHSs located in regional, rural, and remote areas have advised us that better training – tailored to their individual requirements – is needed. As an example, they said they need more training on counselling and supporting victims, given the lack of social workers at their HHSs.
Some, such as the Gold Coast HHS, have sent limited staff to attend the training because their staff hold postgraduate qualifications in clinical forensic medicine. As such, they already have the knowledge, skills, and experience to perform forensic medical examinations, interpret injuries, and prepare expert evidence for court. It also delivers its own forensic medical examination training to its staff.
Queensland Health has advised that it will deliver more training in regional, rural, and remote areas. It plans to deliver training in the Torres and Cape HHS area in October 2024.
Recommendation 2 We recommend Queensland Health ensures suitably trained forensic medical examiners are available across the state to provide timely forensic medical examinations to victims of sexual assault. This should include:
|
Queensland Health has introduced more reporting options for victims and new forensic medical examination kits
In Delivering forensic services (Report 21: 2018–19), we found victims had to report their sexual assault to police before they could undergo a forensic medical examination. We highlighted that this may add to their distress. A victim who has experienced a traumatic event like a sexual assault may be uncertain about reporting the assault to police. They may need time before they can decide.
In July 2019, Queensland Health changed its reporting process, allowing victims to undergo a forensic medical examination without making a formal complaint to police.
In June 2023, it made further improvements, implementing a new collect and store model, allowing a victim to have an examination, with the samples stored at a laboratory. A victim can now choose to make a formal complaint to police at any time up to 24 months after the assault. If they decide to do this, police will notify the laboratory, and it will begin analysing the samples.
New forensic medical examination kits
The Taskforce found the department’s existing sexual assault investigation kits were not appropriate for performing forensic medical examinations. They contained half the number of swabs needed to perform the examination and were inferior to what other states were using.
It recommended that Queensland Health review and update its kits to ensure they are consistent in quality with those used in New South Wales and Victoria. It also recommended they contain DNA decontamination kits and an adequate number of swabs and testing apparatus.
In June 2023, Queensland Health introduced its new forensic medical examination kits. They contain the appropriate contents for a complete forensic examination and for reducing the risk of contaminating forensic samples.
All of the HHSs we audited reported that they have a good supply of kits and that there were short turn‑around times to obtain more kits.
Monitoring the costs and benefits of the new kits
Queensland Health has not monitored the cost of rolling out the new kits across the state. Nor has it assessed the benefits. For example, it does not know whether the new kits are resulting in better quality forensic samples. The laboratory does not provide any feedback to forensic medical examiners on the quality of samples taken.
HHSs advised us that this type of feedback would be valuable in improving practice. Queensland Health is working with the Department of Justice and Attorney-General to develop a way of communicating this information back to HHSs.
Recommendation 3 We recommend Queensland Health improves its monitoring and reporting of the performance of HHSs in delivering forensic medical examinations to victims of sexual assault. This should include:
|